Novel laboratory grown blood vs Naturally synthesized type: which is better?
This would probably be the concluding part of my discussion on regenerative medicine and cellular reprogramming. The discussion today will be aimed at comparing between a naturally synthesized substance in-vivo such as the blood cells with that those produced in-vitro (mainly inside a culture bottle in the laboratory). There is a lot to be discussed but for now, my major focus is on red blood cells because of the critical role they play in our lives.
Laboratory grown blood cell
The basic most interesting biochemistry and function of blood you probably did not know
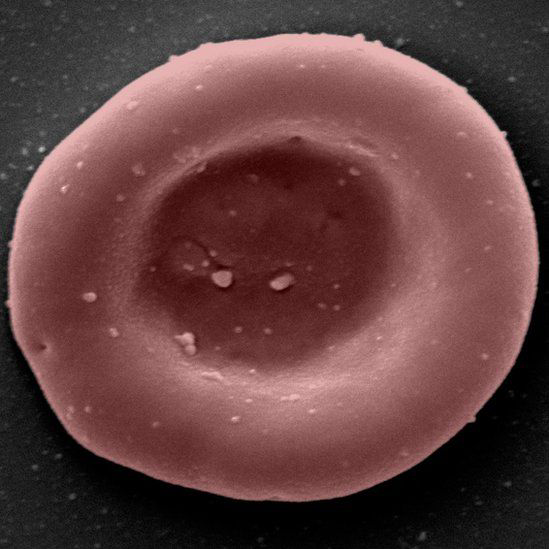
The primary function of red blood cells aka (erythrocytes) is to carry oxygen to the tissues and to return carbon dioxide from these tissues to the lung for oxygenation. They contain haemoglobin molecules to which the oxygen binds and they are mainly responsible for the transportation of this oxygen molecule to tissues and organ in the body. Each molecule of adult haemoglobin (HbA) is made up of four polypeptide chains of globin, 2Alpha chain and 2Beta chains with each chain having its own haem pocket.
Interestingly, the chains of these globin molecules interact and slide with one another during oxygenation and deoxygenation. During deoxygenation, these chains of the globin pull apart or separate thereby allowing the entry of a molecule called 2,3-diphospoglycerate (2,3-DPG) which is responsible for regulating the affinity of these haemoglobin towards oxygen. Their presence automatically reduces the affinity of haemoglobin towards oxygen and vice versa. Without oxygen and haemoglobin interaction, oxygen cannot be delivered to cells, tissue and organs.
why some sickle patients have mild crisis
There is a reason why 2,3-diphospoglycerate must must be present in blood. If 2,3-diphospoglycerate molecules are not present in the blood, haemoglobin will not release oxygen to tissues and organs that need them, this can cause tissue hypoxia (oxygen deprivation of tissues) and necrosis (pathologic cell death in tissues). What will now be the essence of having enough amount of oxygen store, and yet, the major tissues and organs that need them are not receiving them for optimal use. So in essence, it means that its moderate presence ensures that oxygen is released to tissues.
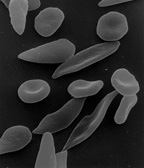
In a situation where the concentration of these 2,3-DPG is higher than normal, oxygen is easily given off, for example in sickle cell anaemia. This is one of the reasons why most sickle cell patients always gasp for air at any slightest oxygen reduction or during activities that would require adequate oxygen use. Though the major reason for lack of oxygen retention by the blood of sickle cell patients is due to the sickle shape of their blood.
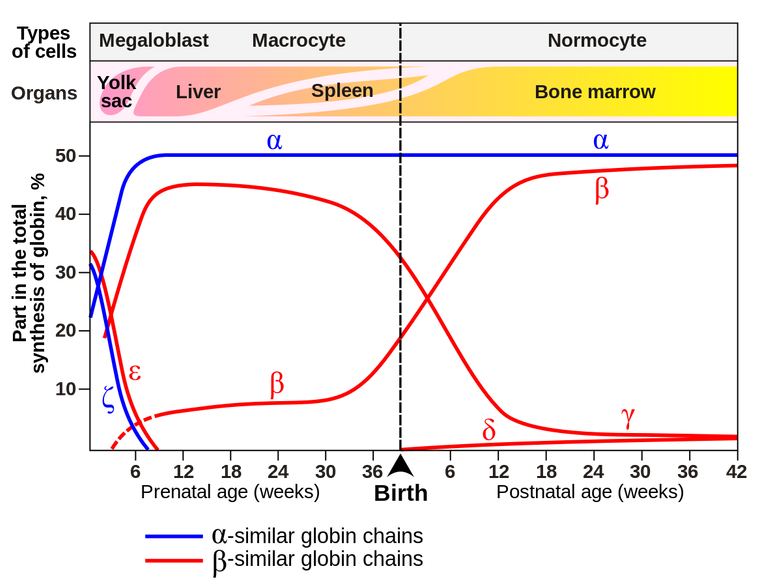
Postnatal genetics
When it comes to children, the reverse is the case. Children below the age bracket (3-6 months) are referred to as fetus. The type of haemoglobin in their blood is called Fetal haemoglobin (HbF). This haemoglobin F (HbF) which contains 2 alpha (α) and 2 Gamma (γ) chains, does not bind 2,3-DPG and thus makes it very difficult for the haemoglobin molecule to give off or release oxygen easily.
You may have ever wondered why episodes crisis differ in some sickle cell patients, some may have mild crisis while some may have severe types. The reason partly because of variation in the amount of fetal haemoglobin in their blood.
As we matured in age, most of the fetal haemoglobin in us are gradually replaced with matured adult haemoglobin molecules. In some people, the case is different. Some people can still have large quantity of these fetal haemoglobin in their blood circulation, and as a result, if it happens that the individual is a sickler, then this will be an advantage for the individual because, their blood would not always easily give up oxygen.
Increasing the body's production of fetal hemoglobin is used as a strategy to treat sickle-cell disease
Now, probably you did not know the main reason why carbon monoxide is extremely dangerous. Yes we all know that it is not good, but the main question is why and how dangerous is it. We will explain that in a matter of seconds. Read on!
The power of carbon monoxide is far greater than that of oxygen in binding to haemoglobin
Carbon monoxide (C0) binds reversibly to haemoglobin in a very stable form and in the process forms carboxyhaemoglobin. It easily displaces oxygen from haemoglobin and consequently makes oxygen unavailable for the haemoglobin. The bond formed between carbon monoxide and haemoglobin is 200 times stronger than that formed between haemoglobin and oxygen.
The above is the reason why when you inhale carbon monoxide accidentally through for example, exhaust fumes from vehicles, you shock, suffocate and gasp for air. Thus, your rate of breathing is increased in order to take in enough oxygen that will replace those displaced by carbon monoxide from the haemoglobin. You are simply paying for what you owe by increasing the rate of respiration, and this is called oxygen debt. I have long prepared a detailed article for you on this topic free which some of the information above were extracted, you can read it here for other information that may interest you, its a very old article. However, this one is more detailed and better explained.
Now you understand the very important role blood plays in our body, let's then compare both the naturally produced types with the ones produced in the laboratory. Hopefully, we may find something interesting. Hey but wait, permit me to ask you first. What are your thoughts, do you think the laboratory grown ones will be better than the natural ones or the natural will be better than the laboratory grown types? While you ponder on that, let's do the comparison, shall we!
Comparing the natural blood vs the lab. grown ones
The search for blood substitute did not start today, in fact, it is a quest that dates back since 1854 when milk was first used as a blood substitute. The idea was that injecting milk helped the patients in need to regenerate more white cells. Other substitutes that were also tried included saline solutions (made from salt concentrate), haemoglobin, plasma, ringer's solution (made up of sodium, potassium, and calcium salts). However, all these proposed substitutes still were not but without some shortcomings. Till date, it is very difficult to find a perfect replacement for natural blood in humans.

Laboratory grown blood
For the record, artificial blood do not totally have the full functions of natural red blood cells, they are mainly produced to carryout one of the most important functions, and that is the transportation of oxygen and carbon dioxide around the body. So they are not entirely produced to replace natural blood in the real sense. The main intent of their production, is to supplement the efforts of natural blood or to aid patients that may be needy of blood but has no other alternative due to incompatibility to many natural blood.
Incompatibility to blood donation by recipients can arise due to many factors. Well, I wouldn't want to talk about them here, fee free to read this lovely article I have crafted for you long before now. Blood group O . I am sure you will learn alot from that article. Instead of patients relying on frequent blood donation, what if those blood that are very difficult to find are produced, this as the real thoughts of the scientist in UK. The thought prompted them to embark of producing artificial blood.
The first world Clinical trial of the artificially grown blood in the laboratory is currently on and this was conducted by NHS Blood and Transplant (NHSBT) arm of the United kingdom's National health service (NHS) around November 2022. Currently they are monitoring the properties of the artificially transfused blood in the patient with the major aim of finding out their survival rate and possible interactions with body system. Some of the features of an ideal artificial blood includes safety and compatibility, oxygen and carbon dioxide transport, shelf life invitro (when stored) and life span in-vivo (inside the body system).
Natural blood in blood bag for storage
Unlike the natural blood which can be stored for not more than a month inside a blood bag contain anticoagulant, artificially produced blood can be stored for longer period of time ranging from months to even years provided the storage conditions are adequate. However, the question is, what will likely be the state of the cells when they are finally transfused into the patients. One thing is common with cells, over time, they degrade or decline in functions.
So for now, we cannot completely assert that artificially produced blood are better m better than natural blood until it is proven beyond reasonable doubt. Health risk and safety concerns are two of the major concerns that has limited the wide acceptance of artificially grown blood. The production of artificial blood in the laboratory do share one thing in common, and that is the need for pluripotent stem cells, in this case, the haematopoietic stem cells which is the progenitor cell for blood cells.
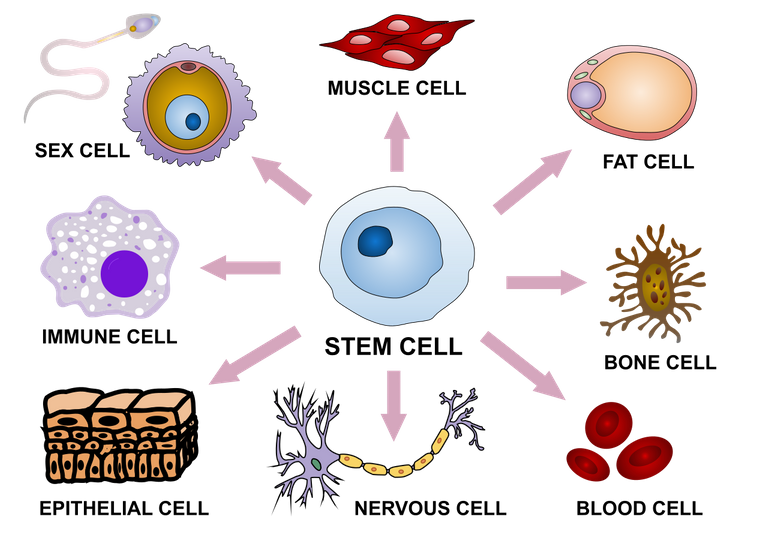
Stem cell differentiation into various tissue types
The scientist in UK took a similar approach but with a bit of twist in terms of hoe they isolated the stem cells. By convention, you can produce artificial blood in the laboratory using three different methods such as synthetic production, chemical isolation, or recombinant biochemical technology. The recombinant DNA method involves reprogramming the cells through pluripotency induction. We have discussed this technique in details in my previous article. You can read them here. It is important to note that, the type of artificial blood you that will be obtained mainly depends on the method you use.
Their method didn't really seem complicated, all they needed was the extraction of the stem cells from the donors.
They start with a normal donation of a pint of blood (around 470ml).
•Magnetic beads are used to fish out flexible stem cells that are capable of becoming a red blood cell
•These stem cells are encouraged to grow in large numbers in the labs
•And are then guided to become red blood cells
The process takes about three weeks and an initial pool of around half a million stem cells results in 50 billion red blood cells.
These are filtered down to get around 15 billion red blood cells that are at the right stage of development to transplant.
There isn't really much complexity in the process. Provided the nutrients, growth factors and necessary conditions such as temperature and other physiological conditions are met, the cells will grow in the cell culture plates like every other cells. However, blood cells cannot be cultured on adherent surface but in cell suspension mediums. They can flocculate and this can result to death of these cells. They always remain in suspension, hence the need for a shaker.
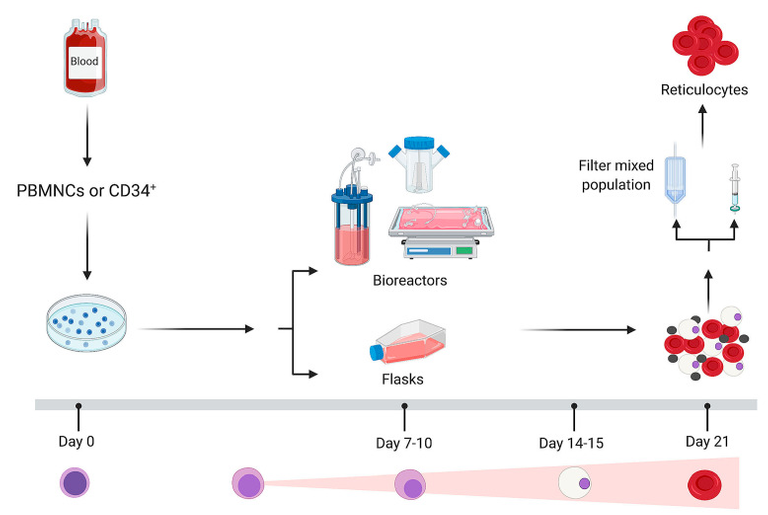
Overview of the erythroid culture process.Ex vivo culture systems require the isolation of peripheral blood mononuclear cells (PBMNC) or magnetic sorting of the CD34+ cells as starting material.
Besides the recombinant DNA technology method, substances like perfluorocarbons (PFCs) have also been tried but were unsuccessful due to one major factor - solubility. PFCs are not soluble in polar solvents and as a result, this makes them quite difficult for use even though they can dissolve oxygen 50 times more than blood plasma. Their inability to react with polar environment makes them unsuitable for use even though efforts have been made to make them interact with non polar environment.
Artificially synthesized Haemoglobin have also been tried, but still with a failure due to the fact that they are unstable and can easily break down and form toxic products in the body system. Some of the haemoglobin are also gotten from expired blood bags. Though they are able to bind oxygen, their instability is a big issue. If the clinical trial by the scientist in UK is a success, it will indeed be a remarkable breakthrough in blood transfusion medicine and of course a relief for patients suffering from hereditary disease like sickle cell anaemia and others.
Based on all of the above and inconclusive evidences, it is very difficult to really infer that artificially produced blood are better than natural types. So, since the natural blood carry out the basic functions as required, they are sure better than laboratory grown artificial types for now until proven otherwise.
That will be all will be all for today. I will keep you informed of a any significant progress and success in the clinical trial.
Do have a great day ahead.
References
•Exploring the biochemistry of glycated haemoglobin HbA1C formation and analysis using the advanced HbA1c analyzer
•First ever clinical trial of laboratory grown red blood cells being transfused into another person
•Blood in a dish: In vitro synthesis of red blood cells
•Artificial Blood: The History and Current Perspectives of Blood Substitutes
•Indian Journal of Critical Care Medicine : Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine - Artificial blood
•Towards manufactured red blood cells for the treatment of inherited anemia
•Artificial Blood Substitutes: First Steps on the Long Route to Clinical Utility
❤️
I actually get excited when I see your writeup because then I know I am going to have a crush course on about 3 or 4 courses I did back in school, and true to my thoughts I get refreshed anytime I read and most often than not I learn a lot of new things.
I love how you present your work, how you go ahead to break down how blood work looking at why sicklers go into crisis when oxygen amount in the atmosphere and available to the system go down, and then one of the interesting things about carbon monoxide which helps us to understand why keeping the car engine on for long whiles staying in the garage could literally end up killing.
Artificial blood has really come a long way and while it is not an absolute replacement for natural blood it has saved a lot of lives and made it possible for surgeons to complete some surgeries and so I am optimistic about the beauty that science holds for us in terms of health and the future. It was a beautiful read, thank you for this.
It's just a matter of time, I am confident there will be a huge breakthrough.
Thank you for the soul suiting compliment.❤️
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
Thanks for including @stemsocial as a beneficiary, which gives you stronger support.
❤️
Yes, better to err on the side of natural until proven otherwise.
For sure...
The devil you know is better than the angel you don't know.