Original Research: Determination of Rubella Virus Infection in Women of Child Bearing Age in a Northern State in West Africa
Today I will be sharing another research work here. This research is mainly about the less commonly heard virus that has been overlooked so far. Though infection by this virus can be prevented through vaccination, having updated statistics on its presence is very necessary because it will help guide epidemiologists, and governmental and non-governmental agencies in making health rules, regulations, and policies.
 Infant with skin lesions from congenital rubella
Infant with skin lesions from congenital rubellaWe will begin with a brief introduction to this virus which is also referred to as the German measles (because it was mostly and closely studied by the Germans in the 19th century) and why it is of economic importance but before we go further, let's have a glance at the entire research work through the abstract.
Abstract
The determination of rubella IgG antibody among two hundred and seventy-two (272) women of childbearing age in Vom was carried out, using the Immune – ELISA rubella IgG quantitative test kit. Seventy–two (72) specimens came from non-pregnant women while 200 specimens came from pregnant women. Out of 72 blood specimens from non-pregnant women investigated, 66 (91.67%) were positive for rubella IgG antibody while 169 (84.50%) were positive out of 200 specimens from pregnant women. Rubella IgG antibody was detected in all the age groups of the women. The women's age ranges from 18-45 years and had no previous history of rubella vaccinations. Among the age groups ages, 21-25 years had the highest rubella antibody (36.11%) in the non-pregnant women while ages 26-30 years had the highest rubella antibodies with 30.00%. in pregnant women. The least rubella antibody among the non-pregnant was 9.72% in ages 31-35 years while it was lower in ages 41-45 with 1.00% in pregnant women. On parity, 1-2 had the highest positive rubella antibodies in both non-pregnant, (38.00) and pregnant women (34.72%) while 11-12 had the least in non-pregnant (1.00%) and 7-8 in pregnant women with 12.50%. the study has shown that a significant proportion of the women have been naturally exposed to rubella virus infection and are therefore immune for life. Rubella virus infection, a disease of medical importance, should be given serious attention. Based on the findings of this study it is strongly recommended that all females before childbearing age should be vaccinated against
rubella.
Keywords: Rubella, Rubella virus, women, pregnancy
Introduction
Rubella virus infection in humans is a global public health problem, especially in developing countries where women of childbearing age are not often vaccinated and are susceptible to the rubella virus. Infection with this virus may result in congenital defects and hence why the concern. It is mostly transmitted from one person to another when the infected person cough or sneezes.
Rubella is caused by the rubella virus, a single-stranded, positive sense RNA virus with envelope glycoprotein spikes. It is a member of the genus rubivirus in the family of Togaviridae. Epidemiologically, rubella is a worldwide human disease and it is endemic in virtually all congenital rubella syndromes. Over 40% of infected persons fail to develop symptoms while about 30,000 cases of congenital rubella syndrome have been documented.
The early onset asymptomatic nature of the viral infection makes it likely dangerous. You won't know until when it probably must have caused some serious damaging effects. Infections that do not present symptoms early enough require proactive measures to curb them and the best and easy way to detect them on time, is to do screening tests for all patients. Since women are also affected and considering how susceptible they are to infections and the deleterious effects the infection might have on developing foetus, it will not be out of place to use them for the study.
The disease is characterized by abortion, stillbirth, rash, mild upper respiratory symptoms, low grade, fever with arthralgia (joint pains), and arthritis (inflammation of the joint in humans) common in young adults as the disease progress.
 Rubella skin rash
Rubella skin rashDuring infection, the evidence of IgM antibody (produced as a result of infection) is diagnostic in recent infections while IgG is considered for immunity due to natural infection in vaccinated susceptible young women or due to vaccination. Generally, antibodies are produced against any foreign body. The type produced and seen in the blood will give you an idea of the infection status - recent or chronic.
This study was designed to primarily determine rubella virus infection among women of childbearing age and our focus was on Vom, a town situated in Plateau State, North Central Nigeria.
The Research methodology
Samples collection and preparation: Blood serum specimens were collected from women of childbearing age, between the ages of 18-45 years. Seventy–two (72) specimens came from no-pregnant women while 200 specimens were obtained from pregnant women. A total of 272 specimens were collected by vane puncture, allowed to clot, and serum separated by centrifugation at 2500 rpm for 10 minutes. The sera were heat inactivated at 560C for 30 minutes in a water bath and kept at – 200C ready for use.
Sample laboratory analysis: The presence of rubella virus antibody in the samples was determined using immunocomb II rubella IgG and IgM, code 6040062 version 400/E5, format 3 X 12 test kit (organics Ltd, Israel). It is an indirect solid phase Enzyme Immuno Assay (EIA) and a quantitative technique based on the antigen-antibody reaction principle. The test results and interpretations were done according to the manufacturer’s instructions and specifications.
Results and findings
Table 1: Presents the overall distribution of rubella antibodies amongst the two groups of women investigated. The pregnant women had the highest rubella antibody level 73.53% than the non-pregnant women. Although more samples were obtained from pregnant women than non-pregnant women.
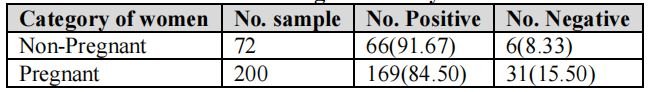
Table 2: The age distribution of rubella IgG antibody among the non-pregnant women is shown in table 2. The results show that ages 21-25 years had the highest rubella antibody with 36.11% while ages 31-35 years have the least (9.72%). However, there were no samples obtained in ages 36-40 and 41-45 years.
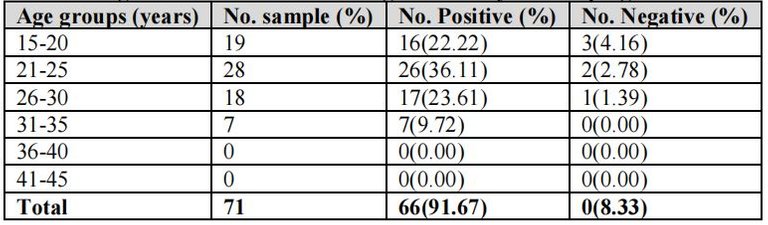
Table 3: Shows the age distribution of rubella IgG antibodies among pregnant women. The result showed that ages 26-30 years had the highest rubella antibody level with 30.00% followed by ages 21-25 years (21.00%) while ages 42-45 years had the least level with 1.00%.
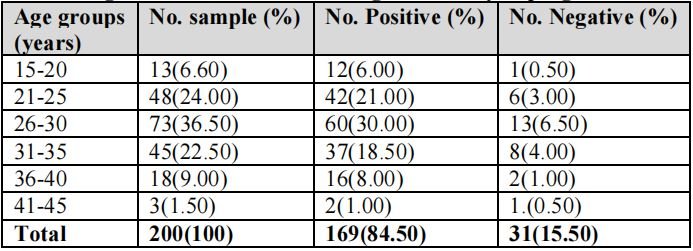
Table 4: The distribution of rubella antibodies based on parity is shown in Table 4. The highest levels of the antibody to rubella were 76 (38.00%) and 25 (34.72%) in non-pregnant and pregnant women respectively and decreases as the parity increased from 1-2 to 11-12. The least were 2 (1.00%) and 9 (12.50%) among the non-pregnant and pregnant respectively.
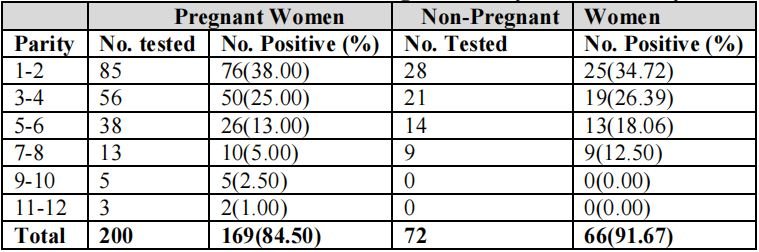
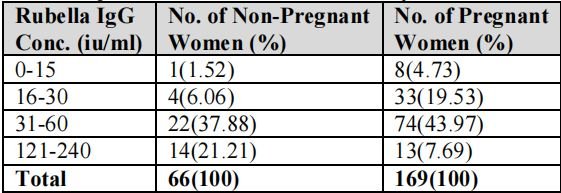
Table 5: Shows the distribution of the subjects based on the concentration of the rubella IgG antibody in their test serum. More women in the non-pregnant childbearing category had their rubella antibody concentration between 31 to 120 IU/ml. Also among the pregnant women of childbearing age, more women had their rubella antibody concentration within 31-12iu/ml. Pregnant women had more women (41) than non-pregnant women in the 0-30iu/ml concentration of rubella antibody.
Discussion
Human infection with rubella virus is one of the major public medical health problems, especially in susceptible women of childbearing age, and has the tendency to cause abortion, stillbirth, and many other major complications in foetuses and neonates. Evidence of rubella virus infection and congenital rubella syndrome has been documented in Nigeria.
In this study, 91.67% prevalence of rubella antibody was obtained from non-pregnant childbearing age women and 84.50% prevalence rate from pregnant women. These results were higher than the rubella haemagglutinating inhibition prevalence rate of 67% reported by Ezeronye, (1985) in Imo State and the ELISA rubella IgG antibody prevalence rate of 77% reported by Onyenekwe and colleagues, (2000). It is also higher than the 73.50% and 79.30% prevalence rates obtained from Adamawa and Kaduna States respectively and 57% prevalence recorded in Makurdi as seen in table 1.
The age distribution of rubella antibodies showed that ages 21-25 years had the highest prevalence rate (36.11%) among the non-pregnant and ages 26-30 years had the highest with 30.00% in the pregnant of the childbearing age women. The least prevalence rates came from ages 31-35 years (9.72%) and ages 41-45 years with 1.00% in non-pregnant and pregnant women respectively (Table 2 and 3).
On parity, the rubella antibodies were the highest in 1-2 with 3800% in pregnant and 34.72% in non-pregnant women (Table 4). The prevalence rates decrease as the parity level increase from 1-2 to 11-12. The distribution of subjects was based on the rubella antibody concentrations in women's serum. The predominating rubella IgG concentrations were 31-60 and 61-120 IU/ml in both non-pregnant and pregnant women of childbearing ages.
However, 14 non-pregnant and 13 pregnant women had their rubella antibody concentrations in 121-240 IU/ml. This could be attributed to the period during which the rubella virus was acquired. The influx of people with very close interaction, lack of awareness of the disease, refection, poor vaccination program, poor rural medical facilities, many below the poverty level, and the availability of susceptible women may be responsible for the spread and maintenance of the disease in the State.
The higher prevalence rates obtained in this study may be attributed to the ELISA test technique used in the laboratory assay, which is more sensitive and specific compared to the haemagglutinating inhibition and single radial haemolysis used by previous workers which are less sensitive.
Some of the recent infections observed among the women may have occurred during child delivery and childhood immunization against rubella, where children are put together in a closed environment and may shed the virus to their susceptible mothers. Sometimes the disease condition may occur due to the state of the patient at the one set of infection.
Since pregnancy is a contraindication to the rubella vaccine, it is important to note that pregnant women are not supposed to be vaccinated and pregnancy should be avoided for at least four weeks after receiving the rubella vaccine.
Conclusively, the study has shown that rubella virus infection is present and is circulating among women of childbearing age. To prevent further transmission and spread of rubella infection, adequate vaccination against rubella should be given to women of childbearing age. Commonly the vaccine given is called MMR (measles-mumps-rubella) vaccine. This vaccine offers great protection against this virus effectively.
Our medical facilities in the hospital and medical centers should be improved and very sensitive and modern serological techniques should be introduced in our health centers to ensure early detection of the disease. We wish to recommend that more work be done in all the medical and health centers nationwide to determine the national prevalence.
Remember, you might not really know on time when infected. As much as possible, observe some distance from people you suspect are coughing or sneezing openly with no handkerchief or protection. When you have the opportunity to be vaccinated, please oblige.
Until I come your way again, please stay safe!
References
Rubella (German Measle) three-day rash
Rubella
Viral Infection in Neonates -Rubella Virus
Rubella (German Measles)
PS: Detailed references can be found in the original published. Click here to access the journal.
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
You may also include @stemsocial as a beneficiary of the rewards of this post to get a stronger support.
😍
Congratulations!
✅ Good job. Your post has been appreciated and has received support from CHESS BROTHERS ♔ 💪
♟ We invite you to use our hashtag #chessbrothers and learn more about us.
♟♟ You can also reach us on our Discord server and promote your posts there.
♟♟♟ Consider joining our curation trail so we work as a team and you get rewards automatically.
♞♟ Check out our @chessbrotherspro account to learn about the curation process carried out daily by our team.
Kindly
The CHESS BROTHERS team
❤️
Hello @cyprianj,
This vaccine was not available when I was a child. I do believe I had what was called German measles back then. Nobody else in the family caught it, but since so many people are asymptomatic (according to your discussion), it's likely my siblings did have it but did not show signs. We lived so closely together.
My question for you today is, if a woman is supposed to avoid pregnancy for four weeks after vaccination, doesn't that present a problem in real-life terms? This suggests lack of intimacy for four weeks. Depending on the education level and willingness to cooperate (of both partners), doesn't this present a challenge?
As always,an informative article. Thank you!
You so right with this and yes, it is sure a challenge. It will now depend the decision of both partners to weigh the risk. The short sexual pleasure they can derive or the chances of having a diseased baby, which is preferable. Sure the risk outweighs the reward.
Moreover, it's just for a month, they could as well decide to do a family planning. This will in a way save the baby and also not deny them of their sexual intimacy.
It's a win win situation for everyone. The baby is safe, and couples are happy.
This added a lot lovely conversation to this discussion, thank you so much for the read and also the lovely compliment 💖.