Erythropoiesis - The Formation of Red Blood Cell (Erythrocytes)
Blood and Red blood cell, are words we are familiar with. We must have heard about them in our simple biology class, but do not know the process of how it is formed. Today, I will be discussing the formation of red blood cell in the human body, its lifespan and everything you need to know about the Histology of red blood cell. Without wasting much time, I should begin.
To understand all about the Red blood cell, you need to understand Erythropoiesis. Erythropoiesis is, to put in simple words, the production of red blood cell in the Red Bone Marrow found in flat bones.
Quick Lecture
- Haematopoeisis is the production of cells into the bloodstream.
- Hematology has to do with studying and understanding the blood and blood related diseases.
- Just as I explained Red Bone Marrow above, there is another bone marrow known as the Yellow Bone Marrow, found the the shaft of long bones, which stores adipocytes.
The creation of Red blood cells in the process of Erythropoiesis occur to replace senescent ones, lost cells from blood loss, low oxygen level (Hypoxia), and other causes including health disorders (such as anemia).
Stages in Erythropoiesis
Iron is usually absorbed from food and different supplements in our body, and it is important for oxygen transfers in the body. Iron exists mainly as the heme compound in erythrocytes and in the muscle cells as myoglobin. Iron can be gotten from heme sources and non-heme sources. Heme iron is easily absorbed into the body and makes up more than 10% of the total absorbed iron, while non-heme iron is less absorbed into the body. .
Iron is absorbed in the duodenum by a reductase enzyme known as Duodenal Cytochrome b, changes the absorbed Fe3+ to Fe2+. The Fe2+ is then transported into the enterocytes with H(+) via the Divalent metal transporter 1 (DMT1). IN the enterocyte, Amyloid Precursor Protein (APP) binds with the iron, to become ferritin. The Ferritin Molecule binds together to become Hemosiderin. Ferroportin transports the Fe2+ out of the enterocyte in the circulatory system, and is converted back to Fe3+ through the help of the ferroxidase Hephaestin. With this simple procedure, Iron has been taken from the stomach, to the duodenum and absorbed into the circulatory system. .
When the Iron is out into circulation, it doesn't move freely, it binds with Transferrin, and it is either transported to used for cellular purposes (Hemoglobin, Iron-containing enzymes, Myoglobin), or can be transported to be stored in iron storage proteins (ferritin or Hemosiderin). The iron is being transported to several tissues and organs including the bone marrow, spleen, and liver. . A hepatocyte, in the liver, produces a protein called Hepcidin, which regulates iron absorption via the restriction of Ferroportin. Let's not forget that the liver produces a protein called HFE gene, which regulates Hepcidin production.,.
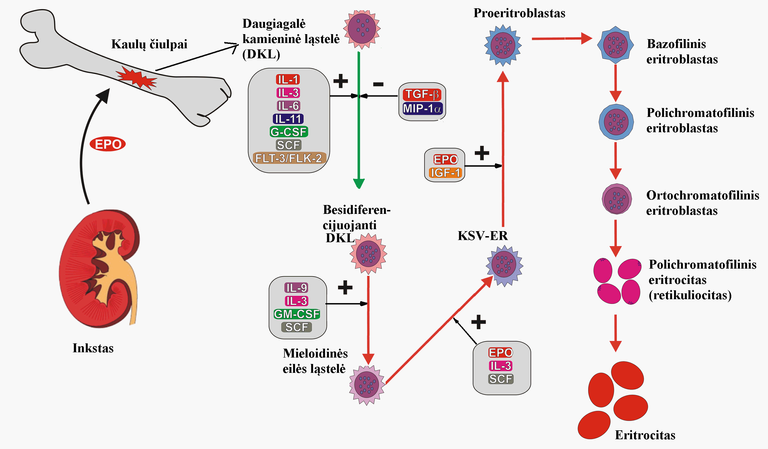
In the bone marrow, there are stem cells for the creation of blood cells called Hemocytoblast / hematopoietic stem cells . These stem cells divides into Myeloid stem cells and lymphoid stem cells. The Lymphoid stem cells create the Lymphocytes which include the T-Cells, B-Cells, and natural killer (NK) cells, but we aren't interested in this. Our interest is in the Myeloid Stem Cells. Myeloid Stem Cells can divide to form platelets, Red blood Cells and White Blood Cells [megakaryocytes and erythrocytes (MegE) as well as granulocytes and macrophages (GM)].
When Myeloid Stem Cells want to produce red blood cells, the Erythropoietin from the kidney stimulates the myeloid stem cell genes to produce Proerithroblast which then starts to create RNAs called Basophilic erythroblasts. The Basophilic erythroblasts are translated to protein polychromatic erythroblast which are immature Erythrocytes. The polychromatic erythroblast translates to become Orthochromatic Erythroblast where the Nucleus and mithochondria, are ejected. The Orthochromatic Erythroblast without a nucleus, known as Reticulocytes, is then ejected from the bone marrow by the Sinusoid capillary into the peripheral blood. The Reticulocytes mature in the peripheral blood into Erythrocytes. .
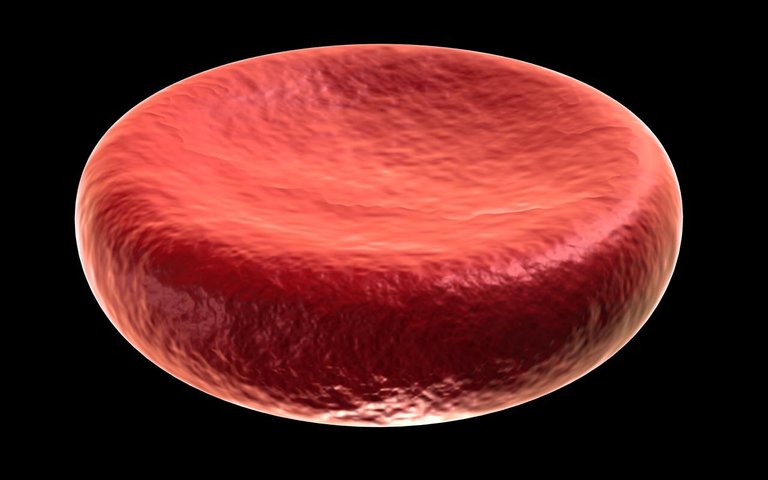
Erythrocyte doesn't have a nucleus or a mitochondrium, which means it cannot utiliaze the oxygen in itself for anything, it is just available for transporting. Erythrocyte, transports Oxygen to the tissues, it transports Co2 from the tissues to the Lungs, and have a short lifespan of 100 to 120 days. In the formation of Erythrocytes, Vitamins B6, B9 and B12 are needed in each of the for the maturation and development of the DNA in the Erythroblasts, and less of them could lead to megaloblastic Anemia, while iron is needed for hemoglobin synthesis. .
Conclusion
The post explains the production of Red Blood Cell (Erythrocytes) which is created in the Red bone Marrow. Iron is very important in the synthesis of Hemoglobin. Not all cells have a nucleus and the Red Blood Cell is one of those cells that do not have a nucleus.
Images
Well written. Erythropoesis is one of the very important processes in the body without which the body won't be able to replace the dead red blood cells after its life cycle. The kidney also plays an important role in the process through the enzyme Erythropoetin, and in most cases of Chronic Kidney Diseases, they present with anamia due to a comprise in the production of this enzyme, erythropoetin.
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
You may also include @stemsocial as a beneficiary of the rewards of this post to get a stronger support.