IOP fluctuations with Glaucoma Medication and Its associated Discomfort
Greetings to all and sundry,
It is a beautiful day today, the end of the week, or the start of a new week depending on how your calendar is arranged either way we are all looking forward to a brand new week and the start of something amazing once again. I wish us all the best.
I do hope that your weekend was fun and full of exciting activities though, well mine was, I got the opportunity to watch Antman and the Wasps, Quantumania yesterday after spending a major part of the day at a friend's wedding. I also used the opportunity, to visit some friends in town.
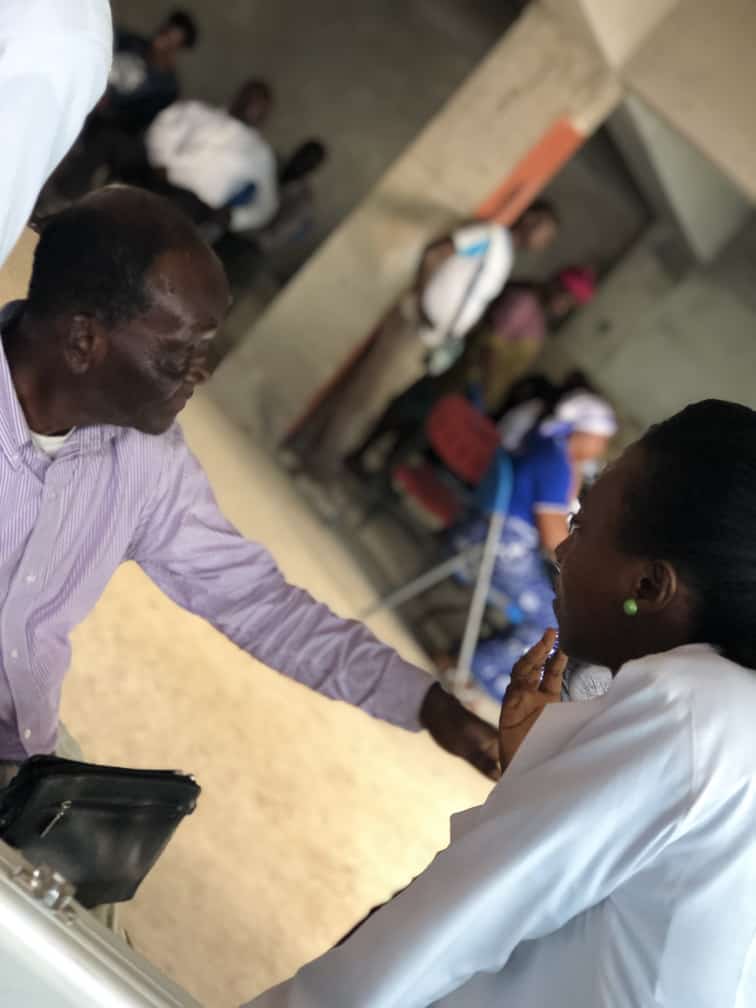
Today, I would be sharing some health tips about glaucoma management and what we ought to do should we find ourselves in that situation. This post was inspired by a recent check-in that came in with my patients and I am hoping that what I shared with them that helped would do you some good too.
Introduction
Glaucoma is a condition that is slowly becoming an African headache with the daily increase in prevalence and incidence, more attention is being drawn to it with the aid of the awareness creation led by the international organization for preventable blindness as well as a wealth of health organization, cooperate bodies and individually owned eyecare firms.
The condition is known as the silent thief of sight because it doesn't give ought any symptoms until the very advanced stages when vision loss is noticed by patients. Symptoms such as headaches that come with very high intraocular pressures such as headaches or ocular pain may easily be attributed to other parameters such as hypertension. Patients are more likely to ignore this unless is extremely severe and only occurs in close-angle glaucoma.

With more research being done about the condition, we still ain't necessarily certain about what causes the condition, there are different schools of thought involving the rise in intraocular pressure killing nerve cells, nerve cells dying idiopathically, genetic implications, etc, however, we still do ain't so certain about the exact cause and the treatment currently focuses on keeping the pressure within the eye within range or a bit lower to reduced.
Like almost every medication used for the treatment of various conditions within the body there are upsides and downsides or should I say possible side effects with drug usage. In the situation of dealing with pressure whether it be systemic or ocular it could go up or go down, either way, the extremes of both could be quite discomforting and so for our discussion today, we would be looking at these two scenarios and what you ought to do when it happens.
Anti-Glaucoma Drugs and Its associated discomfort
One thing that is well-known about glaucoma is its associated rise in intraocular pressure. Note that in low-tension glaucoma this is not the case however it is the case in about 80% of all cases you meet. Now when the intraocular pressure rises the pressure built up pushes against the optic nerve which opens into the brain cavity. As the tension increases ocular structures are stretched out and it becomes discomforting.
You are most likely to experience some pain within the eye as well as increased sensitivity to light. In very extreme cases like acute closure angle glaucoma, you may notice halos around light and you could feel dizzy and nauseous at a point. There are some instances that some have fainted or vomited but these are only in extreme cases.
When this happens it is best to report to the nearest eye care facility, to aid the pain it would be advisable to take some aspirin or paracetamol whiles you find your way to the nearest eye care facility. The extreme cases of IOP rise are considered an emergency and could easily lead to loss of vision within a short time. Once you can find yourself in the hospital you would likely be given oral diamox as well as topical drops to quickly bring down the pressure and save your vision.
If you are a known glaucoma patient then you know that your pressure is only rising because you are not using your antiglaucoma drugs, or you are not using them as instructed by the physician. Now the opposite case of this also does happen, thus when we have our intraocular pressures falling below the accepted range.

This normally happens when we abuse the drugs or dosage as instructed by our physician.. Using a beta-blocker three times daily or four times as opposed to twice daily as it ought to be used could result in this situation or condition. The recommended range is between 11 and 21, plus or minus 2 however when the pressure goes as low as below 8 then it could be very discomforting.
Also, the discomfort and reaction may be idiosyncratic, some people may not necessarily feel much discomfort with a pressure of 8 or 9 however some may not even be able to tolerate 10. When the pressure goes as low as 5 it may be considered hypotony and that would be a dangerous point for the patient and the pressure would have to be elevated quickly.
If you believe you may have used your antiglaucoma medication wrongly and you find yourself with pain, photosensitivity, and headaches after using your drops then it would be advisable that you come in for your Optometrist to help make things better. You could take some aspirin to help things a bit more bearable as you prepare for the clinic.
It is also advisable that you keep hydrated and take in lots of fluids. At the hospital, your Optometrist would most likely recheck your pressure to be certain of what's going on as well as other routine checks. If your pressure is indeed too down, you would most likely be put on steroids for a short while to raise the pressure back to the range after which you would be monitored until it is safe to resume your antiglaucoma medication.
Conclusion
We must follow instructions when it comes to drug usage and does well to report any misuse to our healthcare providers so that we do not find ourselves in any unfortunate situations. Your Doctor is your friend, do not be afraid to come to us when things are not working out for you.
Remember that your vision is your world literally and that you ought to do everything you can to ensure that your site is protected. So do well to have lots of ocular examinations. When in doubt consult a professional and please avoid over-the-counter medication. It was a pleasure serving you today, thanks for reading and for your time
Further Reading
Tran, V. T., Mermoud, A., & Herbort, C. P. (2000). Appraisal and management of ocular hypotony and glaucoma associated with uveitis. International ophthalmology clinics, 40(2), 175–203. https://doi.org/10.1097/00004397-200004000-00014.
Mohan, N., Chakrabarti, A., Nazm, N., Mehta, R., & Edward, D. P. (2022). Newer advances in the medical management of glaucoma. Indian journal of ophthalmology, 70(6), 1920–1930. https://doi.org/10.4103/ijo.IJO_2239_21.
Erb C. (2016). Management von Glaukompatienten [Management of Glaucoma Patients]. Klinische Monatsblatter fur Augenheilkunde, 233(2), 132–133. https://doi.org/10.1055/s-0042-100350.
Leen, M. M., & Mills, R. P. (1999). Prevention and management of hypotony after glaucoma surgery. International ophthalmology clinics, 39(3), 87–101. https://doi.org/10.1097/00004397-199903930-00009.
Thanks for your contribution to the STEMsocial community. Feel free to join us on discord to get to know the rest of us!
Please consider delegating to the @stemsocial account (85% of the curation rewards are returned).
Thanks for including @stemsocial as a beneficiary, which gives you stronger support.
https://leofinance.io/threads/@rzc24-nftbbg/re-nattybongo-u9x66djcxi
The rewards earned on this comment will go directly to the people ( @rzc24-nftbbg ) sharing the post on LeoThreads.